Understanding Sciatica: Causes, Symptoms, and Treatment
Introduction
Sciatica is one of the most searched-for, and most misunderstood, causes of leg pain. Patients often tell me they’re confused by what they read online: some articles say all leg pain is sciatica, while others blame every case of sciatica on a “slipped disc.”
This guide aims to clear things up. I’ll explain what sciatica really is, how it differs from other types of back or leg pain, and why the exact cause matters for recovery. We’ll also bust some common myths and highlight what an effective diagnosis and treatment plan looks like.
What is sciatica?
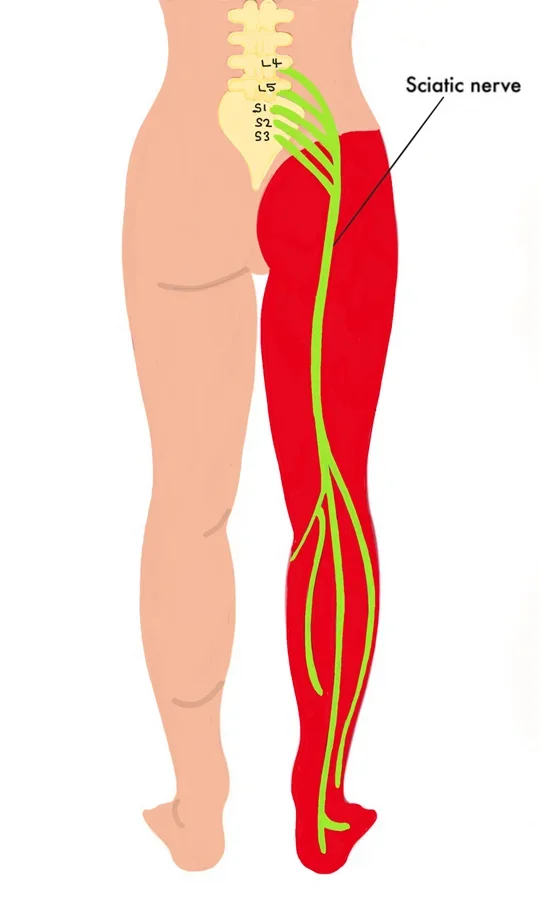
Sciatica is a symptom, not a disease. It occurs when the sciatic nerve or the nerve roots that form it become irritated or compressed. This irritation can happen at the spine or anywhere along the nerve’s path through the buttock and leg.
Because the sciatic nerve travels from the lower back down to the foot, symptoms can appear anywhere along its course, including the lower back, buttock, thigh, calf, or foot.
Key point: Sciatica has multiple possible causes. Understanding the exact source is essential for safe and effective treatment.
Common Causes of Sciatica
A. Nerve root compression in the spine
Disc-related: Bulging or herniated discs pressing on nerve roots.
Joint-related: Stiff or inflamed spinal joints narrowing the space around nerves (foraminal stenosis).
B. Nerve compression outside the spine e.g.
Piriformis syndrome: Nerve trapped in the buttock muscle.
Hamstrings or thigh-level entrapment: Less common, but tight muscles or fibrous bands can irritate the nerve.
Typical Symptoms of Sciatica
True sciatica often affects one side of the body and may include:
Sharp, burning, or shooting pain down the leg
Tingling or “pins and needles”
Numbness or reduced sensation
Muscle weakness (in more severe cases, e.g. foot drop)
Common Myths About Sciatica
Myth 1: “All leg pain with back pain is sciatica.”
False. Pain can come from muscles, joints, or discs without actually involving the sciatic nerve.
Myth 2: “Sciatica always means a slipped disc.”
Not true. While disc problems are common, sciatica can also result from joint issues, spinal canal narrowing, or peripheral nerve compression.
Myth 3: “You always need a scan.”
Most cases can be diagnosed with a careful clinical exam. Scans are only necessary when red flags are present or surgery is being considered.
Myth 4: “Rest is the cure.”
Extended rest often slows recovery. Controlled movement and a guided treatment plan are usually more effective.
Pain That Mimics Sciatica
Not all leg pain that feels like sciatica is caused by nerve irritation. Other tissues—muscles or joints—can create similar sensations. Common examples include:
Discs, joints and muscles in the spine: can create back and leg pain without any irritation of the sciatic nerve
Gluteal trigger points: tight spots in the buttock muscles that refer pain down the leg.
Hip or knee joint problems: pain can radiate to the thighs or calf.
Tight hamstrings or other muscles: producing burning, aching, or shooting sensations.
Key difference: True sciatica usually follows a clear nerve pathway and may include numbness, tingling, or weakness. Pain from other sources is often broader, duller, and less likely to cause neurological symptoms.
How we assess sciatica at Physio7 (Ipswich)
A thorough assessment is key to identifying the cause. Our approach includes:
Functional testing: Observing which movements increase or reduce symptoms—identifying your “directional preference.”
Neurological exam: Checking reflexes, muscle strength, and sensation.
Joint and muscle testing: To spot referred or mechanical pain sources.
Red flag screening: Identifying serious conditions requiring urgent medical attention.
By combining structural (what tissue is involved) and functional (how movements and loads affect it) assessments, we pinpoint the likely cause and guide safe, effective treatment.
Treatment options
Because sciatica is a symptom, treatment depends on the underlying cause. Typical approaches include:
Pain-control strategies: Positions of relief, gentle movement, and education.
Targeted exercise programs: Exercises tailored to your diagnosis, stage of injury, and personal goals.
Manual therapy: Mobilising stiff joints and releasing tight gluteal or spinal muscles.
Neural techniques: Gentle nerve-gliding exercises in selected cases.
Posture and movement retraining: Teaching safe ways to sit, lift, and move.
Referral options: Liaising with GPs, pain clinics, or spinal specialists if symptoms persist or red flags appear.
Recovery and prognosis
Sciatica usually takes longer to settle than simple back pain because nerves heal slowly. Recovery depends on the severity of irritation or compression:
Mild cases: Often improve over days to weeks with conservative care.
Moderate cases: May take several weeks to months, especially if the nerve has been significantly compressed.
Severe cases: Can require specialist input or longer-term management.
Case Study: Jane’s Burning Leg Pain
Background:
Jane, a 32-year-old office worker, noticed a burning, tingling sensation running down the back of her left leg. Running, walking, sitting for long periods or stretching her hamstrings made the symptoms worse. She had no lower back pain.
Assessment:
At Physio7, we examined Jane’s spine, pelvis and hamstrings. Gentle nerve tests (slump test and straight-leg raise) reproduced her leg tingling, indicating irritation of the sciatic nerve around the hamstring rather than at the spine. We also found gluteal and hamstring trigger points contributing to nerve compression.
Treatment Plan:
Education & Pain Relief: Jane learned which positions aggravated her nerve and how to modify her sitting and stretching.
Gentle Nerve Glides: She performed seated sciatic nerve ‘sliders’—slow knee extensions with coordinated ankle and neck movements—to encourage the nerve to move freely through the hamstring.
Muscle Release & Strengthening: Soft tissue work on tight hamstrings and glutes, followed by gentle hip, hamstring and core strengthening exercises.
Functional Training: Jane gradually returned to longer walks and light running, monitoring for any tingling or pain.
Outcome:
After three weeks, Jane reported a significant reduction in tingling and burning. By six weeks, she could sit for work without discomfort and had resumed her regular running routine. Follow-up exercises and posture education helped prevent recurrence.
Key Takeaway:
Not all sciatic-type leg pain comes from the spine. Careful assessment can identify peripheral nerve irritation, and a targeted program of gentle nerve mobilisation, muscle release, and functional training can relieve symptoms effectively.
Final words
Sciatica isn’t a single problem—it’s a symptom with multiple potential causes. Accurate diagnosis—both structural and functional—is essential for creating a treatment plan tailored to your body, not a generic routine.
If you’re in Ipswich and struggling with leg pain, Physio7 can assess the cause and guide your recovery safely.
Book an appointment with an expert physiotherapist today to start your recovery.