Spinal Discs: How They Work, Get Injured, and Recover
Back pain myths are everywhere
….and few are more misunderstood than the so-called “slipped disc.”
Let’s set the record straight.
If you’ve ever been told you have a “slipped disc,” it’s easy to picture a rubbery pad sliding out from between your vertebrae. The reality is far more interesting — and far less alarming.
Spinal discs don’t fall out of your spine. They’re firmly anchored between the vertebrae. What they can do is change shape under load, bulge slightly, or — if the outer fibres are weakened — herniate, where the inner gel pushes through a tear. Even then, the disc stays in place.
Understanding how discs work, how they respond to stress, and how they can wear or recover can help you protect your back for decades.
What Discs Look Like
Imagine your spine as a stack of bricks. Each disc sits neatly between two vertebrae — a shock-absorbing cushion that allows movement, protects the bones, and spreads the heavy forces your spine handles every day.
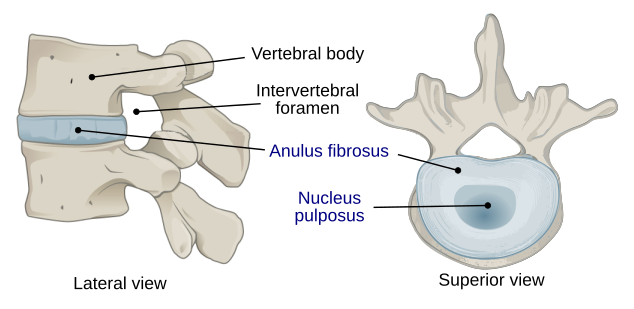
Each disc has three main parts, working together like a high-performance tyre:
Annulus fibrosus — the tyre wall
The tough outer ring made of layered collagen fibres. Each layer runs at a slightly different angle, giving the disc the ability to resist twisting, pulling, and bending without tearing.Nucleus pulposus — the gel filling
The gel-like centre that redistributes pressure when you move, lift, or twist — acting as a natural shock absorber.Endplates — the anchors to bone
Thin layers of cartilage and bone that attach the disc to the vertebrae above and below. They also allow nutrients and waste to move in and out — vital because discs have little direct blood supply.
Attribution: Jmarchn, CC BY-SA 3.0 <https://creativecommons.org/licenses/by-sa/3.0>, via Wikimedia Commons
Discs don’t work alone. Facet joints at the back of the spine act like guiding rails. They help control how much each vertebra moves and share load that would otherwise go entirely through the discs. Their orientation matters: in the lower back, they allow bending and straightening but resist twisting; in the upper back, they allow more rotation.
Why Nature Made Discs This Way
You might wonder: why not have ball-and-socket joints, like the shoulder or hip?
Ball-and-socket joints would be impossible to coordinate for dozens of vertebrae stacked together.
Discs allow controlled twisting and bending across multiple levels.
Discs also act as shock absorbers, distributing forces from your arms, legs, and torso safely across the spine.
How Disc Structure Influences Performance
Collagen Composition
Not all collagen is equal:
Type I collagen — primarily in the outer ring; resists tension and tearing.
Type II collagen — primarily in the inner gel; resists compression and absorbs load.
Other collagens (III, V, VI, IX, X, XI) — link the two systems, fine-tuning stiffness, elasticity, and repair.
Your genetic balance of collagen types partly determines whether your discs are naturally better at bending, absorbing load, or a mix of both.
Disc Shape and Thickness
Lima-bean-shaped discs are strong under compression.
Ovoid discs allow more bending and twisting.
Thicker (“plump”) discs add space between vertebrae, increasing flexibility of that segment. However, added motion may increase the likelihood of strain under repeated bending.
How Discs Can Wear or Get Injured (Flat Tyre Analogy)
Even though spinal discs are tough, repeated stress, age-related changes, or small injuries can gradually affect how they work — much like a tyre that slowly loses air or develops weak spots.
Endplate changes / early degeneration — Tiny fractures in the bony endplates reduce the flow of nutrients into the disc.
Dehydration and softening — The gel-like centre (nucleus) loses water and pressure, becoming more like a soft, underinflated tyre. It still functions, but less efficiently — the load is spread unevenly, and the outer ring works harder to contain it.
Fibrosis and fissuring — Small cracks develop in the annulus (outer ring), making the disc less springy and more vulnerable to strain — like a tyre wall developing weak spots.
Loss of disc height — Similar to a flattened tyre, spacing between the vertebrae shrinks, forcing the facet joints together. This can lead to wearing of the facet joints.
Bulging or herniation — The weakened outer ring may bulge outward, much like a flat tyre spreading under load. In some cases, the inner gel pushes through cracks in the annulus — a true herniation. Crucially, the disc stays anchored — it doesn’t slip out of the spine.
Segmental instability — A healthy, plump disc keeps the spinal “guy ropes” (muscles and ligaments) taut, giving the segment firm control. When the disc softens, those guy ropes slacken, allowing excess movement between vertebrae — which stresses joints, ligaments and nerves.
Segmental stiffness — Over time, as the disc dries and stiffens further, the movement often reduces again, stabilising the segment but at the cost of flexibility.
Key points:
Disc bulges and herniations almost always develop in discs that have already experienced some wear or micro-damage.
Most degenerative changes are normal adaptations and don’t automatically cause pain.
Most painful disc bulges calm down within weeks or months. Over the years, the disc naturally dries and stiffens, which further stabilises the spine and reduces the risk of repeated irritation.
Even discs with degeneration or bulges can remain functional for decades with careful movement, loading, and posture.
What MRI Scans Really Show
MRI scans can be incredibly detailed — but they often tell only part of the story.
Research has repeatedly shown that many people with no back pain at all still show significant disc bulges, herniations, or degeneration on their scans. In fact:
Studies have found that over half of adults in their 30s have visible disc bulges, even when they’re completely symptom-free.
Even elite athletes — rowers, footballers, gymnasts — often show “severe” changes such as disc dehydration or narrowing, yet perform pain-free at the highest level.
So while an MRI can reveal the structure of your spine, it can’t always tell us which changes are actually causing pain. There’s often a poor correlation between MRI findings and symptoms. A disc that looks badly worn may be painless, while a “normal”-looking one might be the real source of irritation.
That doesn’t mean scans are useless — far from it. MRI is very helpful when:
Symptoms are severe, persistent, or unusual.
There’s suspicion of nerve compression or other serious causes.
The findings match your pattern of symptoms and examination results, helping to guide treatment.
The key is context. Scans work best when interpreted alongside a detailed clinical assessment — not as a standalone verdict. The real value lies in connecting the dots between what’s seen on the image and how your spine actually behaves.
Bottom line: MRI findings are a piece of the puzzle, not the full picture. They help confirm what’s going on — but your pain, movement, and recovery all depend far more on function than on the image itself.
Case Study: Adam, the Office Worker
Profile:
Adam, 39, works long hours at a desk. He’d had a nagging ache in his lower back for years, but six weeks before seeing us he developed pain in his right buttock, along with tingling and occasional numbness in his calf and foot.
Problem:
His symptoms were worse when walking, lying on his back, or doing anything that loaded his hips. At first, this sounded like the type of back pain that comes from arching too much — what’s called an extension-dominant pattern. But when we tested his movements, we found that bending forward actually caused the most irritation. His pelvis was also slightly twisted, and several muscles around his hips and spine were out of balance.
My Thoughts:
Adam almost certainly had a minor disc bulge years earlier. To protect himself, he’d slowly stopped bending forward at all. His body adapted — but not helpfully. The loss of flexion left his lower back over-arched and compressed, putting pressure on the joints and nerves instead.
In short, the pain he was feeling now wasn’t just from the original disc problem — it was from how his body had been compensating ever since.
Outcome:
Over six treatment sessions we worked on gently realigning his pelvis, reactivating key muscles, and teaching his spine to move more evenly again. Once his extension bias reduced, his nerve symptoms disappeared, his back pain eased, and he was finally able to get back to lifting weights — something he hadn’t dared to do in years.
After that initial phase, Adam’s back responded much more like a classic “disc” problem. He learned how to load and move safely — using controlled flexion instead of avoiding it altogether. He still needed to be careful not to overdo repetitive or heavily weighted forward bends, but he found a balanced approach that even allowed him to return to deadlifts and squats without pain.
Takeaway from Adam’s Story:
Back pain isn’t always about the disc itself. Sometimes, it’s about how the body compensates around it. Restoring natural movement and balanced control often unlocks recovery when other treatments fail.
Key Takeaways
Discs are living, adaptable joints — built to move and absorb load.
Genetics shape your spine’s makeup and flexibility.
Movement, load, and posture decide how well your discs perform and age.
MRI “abnormalities” are often normal adaptations, not signs of disaster.
With smart loading, varied movement, and attention to control, you can keep your spine strong and pain-free for decades.